Xylazine
Pronounced: zai-lah-zeen
Reading time: 5 minutes
In this post…
What you need to know
- Xylazine has been recently detected in the UK and Scottish drug market. It is a non-opioid sedative and muscle relaxant sold as or found in other drugs like heroin, however more recently ketamine too.
- The effects include sedation, loss of coordination, difficulty breathing, low blood pressure and slowed heart rate.
- Xylazine may slow down heartrate and breathing, so it can be potentially life threatening if mixed with other ‘downer’ type drugs, such as alcohol, opioids, benzodiazepines (Valium, Xanax, etizolam), GHB and ketamine. Xylazine is being sold as or found with some of these drugs, so if you feel unwell, stay with someone and seek help.
- Xylazine is not an opioid, so naloxone is not effective in reversing a xylazine-induced overdose. Naloxone will remain effective against opioids which may have been consumed with the xylazine. If in doubt administer naloxone, but always call 999 as treating an overdose that involves xylazine requires medical care in a hospital setting.
- Xylazine can increase blood sugar levels: complicating its effects on people with diabetes.
- Xylazine has been linked to skin wounds, lesions and ulcers that can become infected, increasing the risk of Blood-borne Viruses (BBVs). If you are concerned, try to speak to a pharmacist, GP or, if you inject drugs, a professional at an Injecting Equipment Provider (IEP) for support.
What is xylazine?
Xylazine has been recently detected in the UK and Scottish drug market. It is manufactured primarily for use as a non-opioid sedative and muscle relaxant. Most often it may be sold as or found in other drugs.
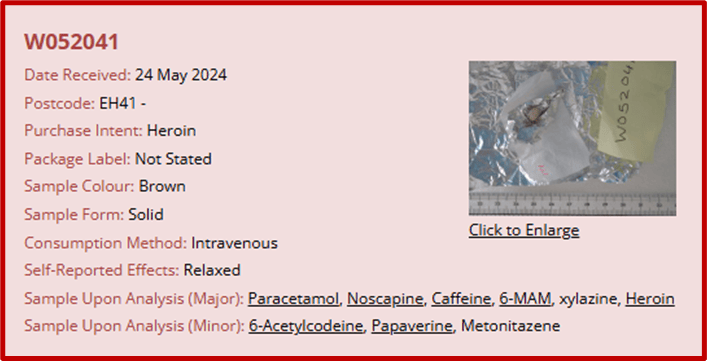
Xylazine has been found in powders (appearing brown, pink or colourless), contaminated heroin, and vape liquid. People who have taken xylazine report: feeling generally unwell, nausea or vomiting, and have reported that xylazine doesn’t smell like heroin and has more of a chemical or even ‘fishy’ smell.
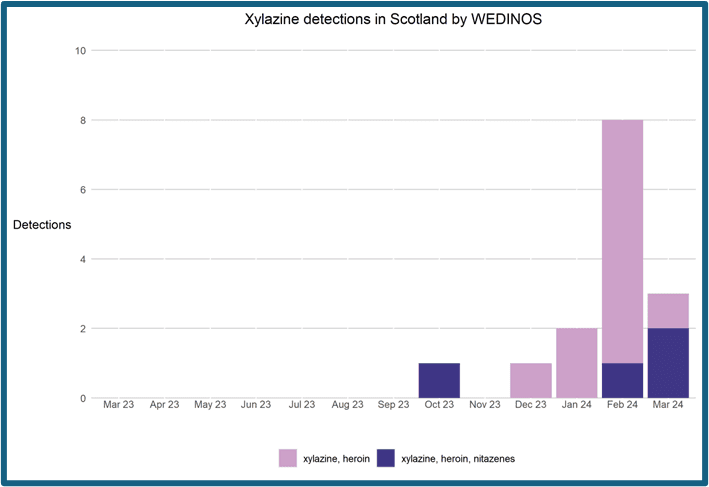
While xylazine was first detected in Scotland in 2020, its current presence has emerged suddenly, and the number of detections continue to increase.
Data by WEDINOS presented by RADAR.
Harm reduction
- Test your drugs – this allows you to be more aware of unexpected contents. Visit www.crew.scot/how-do-i-test-my-drugs for more information on how you can test your drugs.
- Start low; go slow. Begin with a test dose first.
- Try to set timers between doses in a single session to reduce your risk of an overdose.
- Try to avoid mixing drugs, as this may increase your risk of experiencing an overdose.
- If possible, try not to take your drugs alone, and don’t let your mates take them alone either. Stay with a group of people you trust and look out for each other, staying aware of the signs of an overdose.
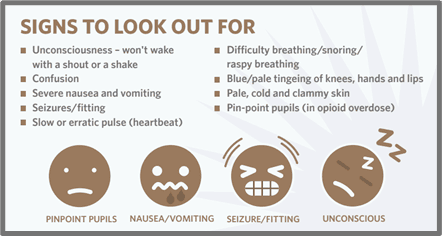
- The signs of a depressant overdose might include:
- Difficulty breathing / snoring / raspy breathing,
- Blue hands, lips or nailbeds,
- Pale, cold and clammy skin,
- Pinpoint pupils,
- Unconsciousness or unresponsiveness.
- Carry naloxone in case of on opioid-related emergency. In Scotland the provision of naloxone is FREE and anyone 16 or over can grab a naloxone kit from the Crew Drop-in or visit www.crew.scot/what-we-do/get-naloxone.
- If you use opioids every day, consider attending a drug treatment service who can prescribe you methadone or buprenorphine. These alternatives will not carry the risk of containing adulterants like xylazine or nitazenes and therefore may reduce your risk of experiencing an overdose.
- Use clean injecting equipment provided by an Injecting Equipment Provider (IEP) to prevent the spread of infections or Blood-Borne Viruses (BBVs).
- Ensure any wounds or ulcerations that you may have are treated properly. Your Injecting Equipment Provider can either provide this care or signpost you to the appropriate service.
In an emergency
- Always call 999 in an emergency.
- Naloxone should be given to anyone who is non-responsive and displaying the signs of an overdose.
- If you are unsure if the person has taken opioids, always use naloxone as this will not cause any harm and could save their life.
- If someone has been taking opioid drugs mixed with other depressant drugs such as xylazine, alcohol or benzos then naloxone will not reverse the effects of these drugs. You should still administer naloxone as this will reverse the effects of the opioids and allow the person’s body the chance to respond to the ‘downer’ effects of any other drugs and could save their life!
Administering naloxone
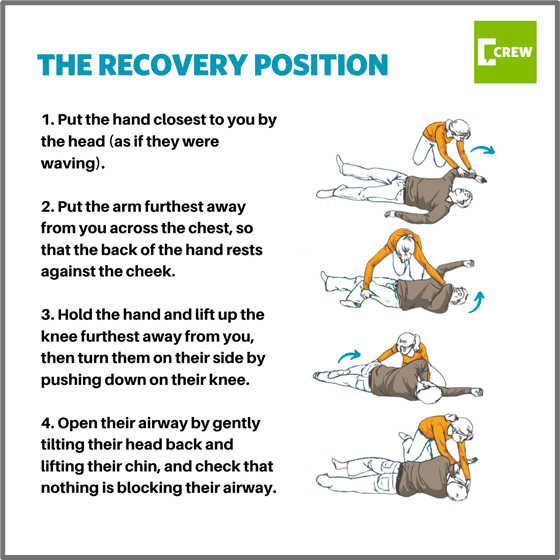
- Put the person into the recovery position if possible (as shown below).
- IM (intramuscular) naloxone should be administered into the muscle at the top of the thigh.
- It can also be administered into the top part of the arm between the elbow and shoulder where vaccines are usually administered.
- If someone has not responded to the first dose of IM naloxone administered into their thigh then a second dose could be administered into the top of their arm to increase the effectiveness of the medicine.
- Remember that you can administer up to 5 doses per injecting naloxone (Prenoxad) kit, and 1 per nasal naloxone (Nyxoid) kit.
- If the person stops breathing perform CPR (chest compressions and rescue breaths) where possible.
- Naloxone does not affect breastfeeding so this should not discourage you from administering it.
- The aim of naloxone is to save a life so if a pregnant person is overdosing and at risk of death, naloxone should be administered.
- Take extra care when inserting the needle if the person has low body fat/muscle mass.
- The person may vomit, be disorientated, dizzy, nauseous, anxious or be aggressive when they wake up.
- The effects of naloxone can wear off after 20-30 minutes so ensure you stay with the person in case they go back into overdose.
References
Recent updates
Following the ACMD report in February 2024, it was recommended that xylazine to be controlled as a Class C under the Misuse of Drugs Act 1971 and inclusion in Part 1 of Schedule 4 to the 2001 Regulations. The Government has accepted these recommendations.
From January 15th 2025, Xylazine will be controlled under the Misuse of Drugs Act as a Class C drug.
This means:
- Possession carries a maximum penalty of up to 2 years in prison and an unlimited fine (or both)
- Production and supply carries a maximum penalty of up to 14 years in prison and an unlimited fine (or both)